DCDC Academy of Healthcare: Your Gateway to a Rewarding Career in Dialysis Technology

In a country where the demand for qualified dialysis professionals is growing exponentially, DCDC Academy of Healthcare emerges as a transformative force, committed to shaping the future of healthcare. Powered by the legacy of DCDC Kidney Care — a trusted network of 200+ dialysis centers across India — the Academy offers a 2-Year Diploma in Dialysis Technology that is not only affordable but also life-changing.
🌟 Why DCDC Academy? Because You Deserve More Than Just a Course
✔️ 100% Job Guarantee – Secure placement upon course completion
✔️ Minimal Fees – ₹75,000 only for Offline & ₹50,000 only for Online Students
✔️ On-the-Job Training (OJT) – 12 months of real-world clinical exposure
✔️ National Recognition – Affiliated with AHPI & IMA
✔️ Offline, Online & Hybrid Modes – Learn from anywhere, anytime
✔️ Easy Instalments – Upto 3 Instalments in initial quarter.
✔️ Special Female Discounts – Uplifting women in healthcare
Diploma in Dialysis Technology: Course Overview
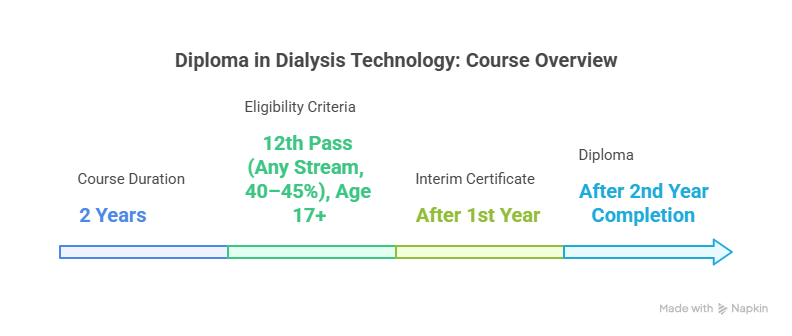
- Duration: 2 Years
- Eligibility: 12th Pass (Any Stream, 40–45%), Age 17+
- Certification:
📝 Interim Certificate after 1st Year (for internal purpose)
🎓 Diploma after 2nd Year Completion
Course Structure:
|
Phase |
Duration |
Key Focus Areas |
|
🧩 Phase 1 – Foundation Learning |
6 Months |
– Human Biology, Anatomy & Physiology |
|
🔬 Phase 2 – Practical Immersion |
6 Months |
– Dialysis Lab Training & Equipment Handling |
|
🏥 Phase 3 – On-the-Job Training |
12 Months |
– Real Patient Exposure in DCDC Centers – Vitals Signs Monitoring |
But what truly sets DCDC Academy apart?
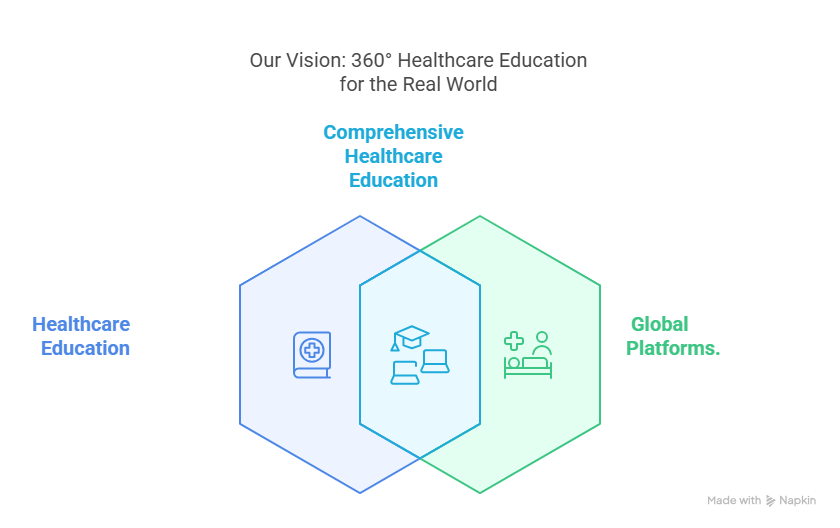
🎯 Our Vision: 360° Healthcare Education for the Real World
At DCDC Academy, education is not just about textbooks. Our vision is to provide students a 360-degree learning experience, preparing them not only as dialysis technicians but as multi-skilled healthcare professionals ready to excel on global platforms.
🧠 Subjects like Soft Skills, Microsoft Office (Word, Excel, PowerPoint)
🦾 AI in Healthcare
💉 BLS & ACLS Training
🍽️ Renal Diet Management
💧 Water Treatment & RO Plant Operations
🩺 Kidney Transplant Coordination & Infection Control
This all-encompassing curriculum gives students a competitive advantage that very few institutes in India offer — and that too at such minimal cost.
💬 Hear it from Our Students
“This course gave me more than just a job—it gave me confidence, real skills, and a purpose. I’m now job-ready, thanks to the expert guidance and practical exposure at DCDC.”
— Sahil Saini, Batch 2
“The curriculum covered everything from patient care to digital tools. I feel confident not just as a technician, but as a true healthcare professional.”
— Aditi Chauhan, Batch 2
Beyond Classrooms: Life at DCDC Academy
DCDC believes that education should be experiential. From lab simulations, hands-on practice, convocation ceremonies, guest lectures to national celebrations — the Academy provides a holistic campus experience that shapes both personality and professionalism.
🌏 Affordable. Flexible. Empowering.
Whether you’re just out of school, looking for a new career path, or dreaming of a stable future in healthcare — DCDC Academy opens the door for all. With both offline and online learning options, special support for female students, and an industry-integrated program, your journey from learner to leader starts right here.
📞 Admissions Open – Join Now!
📍 B-22, Basement, Opp. Metro Pillar No. 225, New Multan Nagar, Paschim Vihar, Delhi – 110056
🌐 academy.dcdc.co.in
📲 Call/WhatsApp: 011-4555 2688 | 89290 67521
📧 Email: academy@dcdc.co.in
🚨 Limited Seats | Career-Ready Curriculum | 100% Job Guarantee
DCDC Academy of Healthcare isn’t just building careers.
It’s building confident, future-ready professionals—Every Student counts.